Are you a nursing student preparing for your first Fundamentals of Nursing Exam? Are you feeling overwhelmed with the amount of material you need to study? Look no further!
In this article, we will provide you with comprehensive study material for your Fundamentals of Nursing Exam 1 in PDF format.
The Fundamentals of Nursing Exam is an essential part of your nursing education, as it covers the foundational concepts and skills required for competent nursing practice. This exam will test your knowledge on nursing theories, the nursing process, health promotion and maintenance, infection control, medication administration, and patient safety.
It is crucial to have a solid understanding of these concepts to provide safe and effective patient care. With our comprehensive study material, you can feel confident in your ability to succeed on the Fundamentals of Nursing Exam.
Key Takeaways
- The Fundamentals of Nursing Exam 1 covers important topics such as nursing theories, nursing process, health promotion and maintenance, infection control, medication administration, and patient safety.
- Understanding these concepts is crucial for safe and effective patient care.
- Nursing theories provide a framework for understanding nursing and guiding decision-making in clinical practice and evidence-based practice.
- Prioritizing patient safety, proper patient identification, and personalized care are important aspects of nursing practice.
Understanding Nursing Theories
You’re going to learn about nursing theories, which will help you understand the foundation of nursing and how it has evolved over time. Nursing theories provide a framework for understanding the art and science of nursing. They are important because they help nurses identify patient needs, plan and implement interventions, and evaluate outcomes.
Understanding nursing theories is also essential for their application in clinical practice. Nurses use theories to guide their decision-making and actions, helping them to provide holistic care and improve patient outcomes.
Moreover, nursing theories provide a basis for research and evidence-based practice, which is crucial in advancing the profession and improving patient care. Therefore, studying nursing theories is not only important for passing exams but also for becoming a competent and effective nurse.
The Nursing Process
When it comes to the nursing process, there are five key steps you should be familiar with: assessment, diagnosis, planning, implementation, and evaluation.
You’ll use these steps to provide the best possible care to your patients. By following this process, you’ll be able to identify any issues, develop a plan to address them, and track your progress along the way.
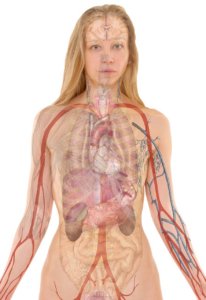
Assessment
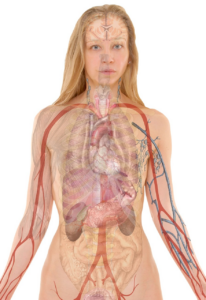
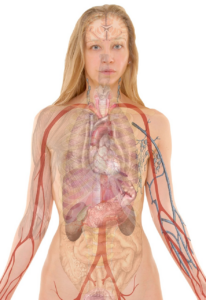
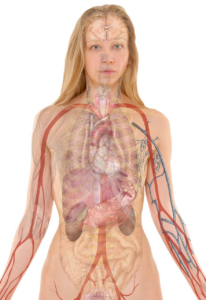
As you begin assessing a patient, it’s important to establish a rapport and create a comfortable environment to encourage open communication. This will help you gather valuable information about the patient’s physical, emotional, and mental health.
During the assessment, you will use various assessment techniques such as inspection, palpation, percussion, and auscultation. These techniques will help you identify any abnormalities or changes in the patient’s health status.
As you perform the assessment, it’s crucial to follow documentation standards. You need to document all the information you gather accurately, thoroughly, and in a timely manner. This documentation will serve as a record of the patient’s health status, progress, and any interventions that were performed.
It’s also important to maintain confidentiality and privacy when documenting patient information. By following these assessment techniques and documentation standards, you can provide high-quality patient care and ensure that the patient’s health needs are met.
Diagnosis
Now that you’ve gathered all the necessary information during the assessment, it’s time to use your clinical judgment to make a diagnosis and determine the best course of treatment for the patient. This is where your critical thinking skills come into play.
As a nurse, you need to analyze all the data gathered during the assessment and identify the patient’s health problems. This will help you create a care plan that addresses the patient’s unique needs.
To ensure that your nursing interventions are effective, you need to follow these four steps when creating a care plan:
- Prioritize the patient’s health problems based on their severity and impact on the patient’s overall health.
- Identify measurable goals and outcomes that you want to achieve with your interventions.
- Develop nursing interventions that are evidence-based and tailored to the patient’s individual needs.
- Continuously evaluate the effectiveness of your interventions and adjust your care plan as needed.
By following these steps, you can provide the best possible care for your patients and help them achieve optimal health outcomes.
Remember, nursing interventions and care planning are crucial components of the nursing process, so take your time and use your clinical judgment to create a comprehensive care plan for your patients.
Planning
To create a personalized care plan for your patient, prioritize their health problems, identify measurable goals, develop evidence-based interventions, and continuously evaluate their effectiveness. Goal setting is crucial in planning, as it provides a clear direction for the care team. Goals should be specific, measurable, achievable, relevant, and time-bound (SMART).
For example, a goal for a patient with diabetes may be to reduce their HbA1c level from 9% to 7% within the next three months.
Care coordination is also an essential aspect of planning. It involves collaboration among healthcare professionals, patients, and their families to ensure that the patient receives the right care at the right time. Care coordination includes communication, information sharing, and ensuring that all healthcare professionals involved in the patient’s care are aware of their goals, interventions, and progress.
By prioritizing health problems, setting specific goals, and coordinating care, you can develop a personalized care plan that meets the unique needs of your patient.
Implementation
Context:
Implementation
Input:
Implementation of the personalized care plan involves putting the identified interventions into action, regularly monitoring the patient’s progress, and making adjustments as needed. It’s important to remember that the implementation stage isn’t just about following a set plan but also about using clinical decision making to determine the best course of action for each patient.
To ensure success during this stage, consider the following implementation strategies:
-
Communicate with the patient: Discuss the care plan with the patient and their family to ensure they understand and are comfortable with the interventions. This will increase compliance and improve outcomes.
-
Use evidence-based practice: Implement interventions that have been proven effective through research and evidence-based practice. This will ensure the best possible outcomes for the patient.
-
Monitor progress: Regularly monitor the patient’s progress to determine if adjustments need to be made. This will ensure that the care plan remains personalized and effective for the patient’s specific needs.
By following these implementation strategies, the personalized care plan can be put into action with confidence and success. Remember to use clinical decision making to determine the best course of action for each patient and make adjustments as needed to ensure the best possible outcomes.
Evaluation
You should evaluate the effectiveness of the personalized care plan to ensure that it’s meeting the patient’s needs and achieving the desired outcomes. Evaluation techniques can include observing the patient’s progress, engaging in open communication with them, and analyzing their medical records. It’s important to document any changes in the patient’s condition and adjust the care plan accordingly.
In addition, a performance appraisal should be conducted to evaluate the nurse’s ability to implement the care plan effectively. This can include assessing their communication skills, time management, and attention to detail. It’s important to provide feedback to the nurse and provide opportunities for them to improve their skills.
By evaluating both the care plan and the nurse’s performance, you can ensure that the patient is receiving the best possible care.
Health Promotion and Maintenance
One must prioritize health promotion and maintenance in order to prevent illnesses and maintain optimal well-being. This involves adopting a healthy lifestyle and taking measures to prevent diseases. A healthy lifestyle includes eating a balanced diet, engaging in regular exercise, getting enough sleep, and avoiding harmful substances such as tobacco and excessive alcohol consumption. Additionally, regular check-ups with healthcare professionals can help detect any potential health issues early on and prevent them from becoming more serious.
In terms of disease prevention, there are various measures that can be taken to reduce the risk of contracting illnesses. These include practicing good hygiene, such as washing hands frequently and covering the mouth and nose when coughing or sneezing, as well as getting vaccinated against certain illnesses. It is also important to be aware of potential health hazards in the environment and take steps to mitigate their effects. By prioritizing health promotion and maintenance, individuals can take control of their own well-being and reduce the likelihood of developing chronic illnesses or suffering from preventable diseases.
| Healthy Lifestyle | Disease Prevention | |||
|---|---|---|---|---|
| Eating a balanced diet | Practicing good hygiene | |||
| Engaging in regular exercise | Getting vaccinated | |||
| Getting enough sleep | Being aware of potential health hazards | |||
| Avoiding harmful substances | Visiting a healthcare provider regularly |
Infection Control
In this subtopic, you’ll learn about types of infections, how they’re transmitted, and the prevention and control measures you can take.
Knowing the different types of infections is important as each requires different treatment and management.
Understanding how infections are transmitted will help you take proactive measures to prevent their spread.
Learning about prevention and control measures will help keep yourself and those around you safe and healthy.
Types of infections
Hey there, let’s dive into the different types of infections, shall we? Infections can be classified in a number of ways, depending on the factors that are considered. One way to classify infections is according to the organism that causes them. Bacterial infections, for example, are caused by bacteria, while viral infections are caused by viruses. Fungal infections are caused by fungi, and so on. Another way to classify infections is according to the part of the body that is affected. Respiratory infections, for example, affect the lungs, while urinary tract infections affect the kidneys, bladder, and urethra.
Prevention measures and treatment options vary depending on the type of infection. Bacterial infections, for instance, can be prevented by practicing good hygiene, such as washing hands frequently and thoroughly. They can also be treated with antibiotics. Viral infections, on the other hand, cannot be treated with antibiotics, but can be prevented through vaccination. Fungal infections can be prevented by avoiding exposure to fungal spores and treated with antifungal medication. By understanding the different types of infections and their prevention and treatment options, healthcare providers can better care for their patients and prevent the spread of infections.
| Type of Infection | Organism | Prevention Measures | Treatment Options |
|---|---|---|---|
| Bacterial | Bacteria | Good hygiene, antibiotics | Antibiotics |
| Viral | Virus | Vaccination | Symptom relief |
| Fungal | Fungi | Avoid exposure to spores, antifungal medication | Antifungal medication |
There are various types of infections that healthcare providers must be aware of. By understanding the different organisms that cause infections and the parts of the body that are affected, providers can tailor their prevention and treatment measures accordingly. Whether it be practicing good hygiene or administering medications, preventing and treating infections is crucial in maintaining the health and wellbeing of individuals.
Transmission of infections
Now, imagine yourself in a crowded room where people are coughing and sneezing, and you start to wonder how infections are transmitted.
There are several modes of transmission that can lead to the spread of infections. The most common modes are contact, droplet, airborne, and vector-borne transmission.
Contact transmission involves direct or indirect contact with an infected person or object. This can occur through touching, kissing, sexual contact, or sharing personal items such as towels or razors.
Droplet transmission occurs when an infected person coughs, sneezes, or talks, and droplets containing common pathogens are released into the air. These droplets can travel up to 3 feet and infect others who come in contact with them.
Airborne transmission occurs when infectious particles are suspended in the air and can be inhaled.
Vector-borne transmission occurs when insects or animals transmit infectious pathogens to humans.
Understanding these modes of transmission is essential in preventing the spread of infections.
Prevention and control measures
Now that you know about the different ways infections can be transmitted, it’s time to focus on prevention and control measures. These are crucial in healthcare settings to ensure the safety of patients and healthcare workers. By following these measures, you can significantly reduce the risk of infections spreading.
One important prevention measure is vaccination. Vaccines are a safe and effective way to protect against infectious diseases. It’s important to stay up to date on your vaccinations and encourage others to do the same.
Another important measure is the use of personal protective equipment (PPE). PPE includes gloves, gowns, masks, and eye protection. Wearing the appropriate PPE can prevent the spread of infections from one person to another.
Remember, prevention is key when it comes to infection control.
Medication Administration
Medication administration can be a bit nerve-wracking, but it’s important to remember to double check everything before giving the medication. Medication errors can be life-threatening, so it’s crucial to ensure that you’re administering the correct medication at the right time and in the right dose. Here are some tips to help you feel more confident when administering medication:
- Take your time and don’t rush through the process.
- Use the rights of medication administration: right patient, right medication, right dose, right route, and right time.
- Make sure to check the medication label against the medication order to verify that it’s the correct medication.
- Verify the patient’s identity before administering medication.
- Keep a medication administration record to track the medications given and the patient’s response to them.
- Always document the medication administration in the patient’s medical record.
Medication reconciliation is also an important aspect of medication administration. It’s the process of creating an accurate list of all the medications a patient is taking, including prescription drugs, over-the-counter medications, and herbal supplements. This list is used to compare the medications the patient is taking to the medications that are prescribed to ensure that there are no drug interactions or duplications.
By performing medication reconciliation, you can prevent medication errors and provide safe care to your patients.
Patient Safety
As a nurse, it’s crucial that you prioritize patient safety at all times. This involves proper patient identification to ensure that the right medication and treatment is given to the correct patient.
Fall prevention measures should also be implemented to avoid any injuries that may occur due to slips or falls.
Additionally, proper use of restraints and emergency preparedness plans must be in place to ensure the safety and well-being of your patients.
Patient identification
Identifying patients correctly is crucial in providing safe and effective care, so it’s important to double-check their name and other identifying information before administering any treatments or procedures. Patient safety is at risk if healthcare providers fail to confirm the patient’s identity, leading to medication errors, wrong procedures, and other potential harm.
To avoid these errors, healthcare providers follow identification protocols that ensure that the right patient is receiving the right treatment. One common identification protocol is the use of wristbands, which contain the patient’s name, hospital number, and other identifying information. These wristbands are checked and verified by healthcare providers before any treatment or procedure is initiated.
Additionally, healthcare providers may ask patients to state their name and date of birth or use electronic identification systems, such as barcodes or radio-frequency identification (RFID) technology, to further confirm the patient’s identity. By following these identification protocols, healthcare providers can guarantee that the patient receives the right treatment at the right time, ensuring patient safety and preventing potential harm.
Fall prevention
To keep patients safe and prevent potential harm, healthcare providers implement fall prevention strategies using a variety of interventions. Falls are a common occurrence in healthcare settings, and they can lead to serious injuries, increased hospitalization time, and even death. Therefore, it’s essential to identify and address risk factors that increase the likelihood of falls.
Risk factors that increase the likelihood of falls include age, history of falls, cognitive impairment, and medication use. Healthcare providers can implement interventions to decrease these risk factors and prevent falls. These interventions include educating patients and their families about fall prevention, conducting fall risk assessments, modifying the environment to reduce fall hazards, and encouraging patients to use assistive devices such as handrails and walkers.
By implementing these interventions, healthcare providers can significantly decrease the risk of falls and improve patient safety.
Restraint use
Restraint use is a controversial topic in healthcare that can have significant physical and psychological consequences for patients. While restraints may be used to prevent falls, reduce wandering, and ensure patient safety, they can also cause harm to patients, including injuries, psychological distress, and loss of dignity. Ethical considerations must be taken into account when deciding whether to use restraints, and healthcare professionals must carefully weigh the potential benefits against the risks when making this decision.
Fortunately, there are alternatives to restraint use that can be implemented to promote patient safety and comfort. These alternatives may include environmental modifications, such as adding handrails or removing clutter, or the use of assistive devices, such as bed alarms or pressure-sensitive mats. Additionally, healthcare professionals can work with patients and families to develop individualized care plans that address specific concerns and needs.
By utilizing these alternatives, healthcare professionals can help to minimize the use of restraints and promote patient-centered care.
Emergency preparedness
Emergency preparedness is crucial in healthcare settings, as it ensures that healthcare professionals are equipped with the necessary resources and protocols to respond to potential emergencies. Emergency response aims to provide immediate and effective assistance to those in need during unexpected events. Disaster management, on the other hand, refers to the process of preparing for, responding to, and recovering from a disaster.
Here are some key points to consider when it comes to emergency preparedness in healthcare:
- Establishing an emergency response team that includes staff from various departments and disciplines
- Developing and implementing emergency plans and protocols that are regularly reviewed and updated
- Ensuring that healthcare professionals receive appropriate training and education on emergency response and disaster management
- Maintaining an inventory of emergency supplies and equipment
- Conducting regular drills and exercises to test emergency preparedness and identify areas for improvement
By taking these steps, healthcare facilities can be better prepared to respond to emergencies and provide the best possible care to their patients and staff. Remember, being prepared is key to ensuring the safety and well-being of everyone involved.
Frequently Asked Questions
What is the passing score for the Fundamentals of Nursing Exam 1?
To answer your question about the passing score for the fundamentals of nursing exam 1, it’s important to consider the exam difficulty.
The passing score for any exam is typically determined by the level of difficulty of the questions and the overall performance of the test-takers.
In some cases, passing scores may be set higher or lower depending on the importance of the exam and the qualifications required for a particular profession.
However, without knowing the specific details of the fundamentals of nursing exam 1, it’s difficult to determine what the passing score may be.
It’s best to consult the exam materials or speak with your instructor to get a better understanding of what score is required to pass.
How many questions are on the Fundamentals of Nursing Exam 1?
So you’re wondering about the number of questions on the fundamentals of nursing exam 1 and the exam format.
Well, the exact number of questions varies depending on the testing institution, but typically the exam consists of around 100 to 150 multiple choice questions.
The exam format usually follows a computer-based testing system where you’ll be given a set amount of time to complete the exam.
The questions will cover a wide range of topics related to nursing fundamentals, such as patient care, communication, pharmacology, and safety protocols.
It’s important to study thoroughly and be prepared for the exam to ensure you pass and move forward in your nursing career.
Is the Fundamentals of Nursing Exam 1 timed?
When it comes to taking timed exams, time management strategies are key. You’ll want to make sure you have a good understanding of the material so you can move through the questions efficiently.
But even if you’re well-prepared, it’s important to stay focused during the exam. Try to eliminate distractions and keep a steady pace. Don’t get bogged down on difficult questions – if you’re stuck, move on and come back to them later.
And remember to take breaks if needed to avoid burnout. With these tips, you can tackle any timed exam with confidence.
Are there any prerequisites required to take the Fundamentals of Nursing Exam 1?
Before taking the Fundamentals of Nursing Exam 1, there are some prerequisite qualifications that you need to meet. These may vary depending on the institution providing the exam, but generally, you need to have completed the relevant coursework and clinical experience. Additionally, you might need to have a minimum GPA or pass specific prerequisite classes.
It’s essential to check with your school or program to determine the specific requirements. Exam preparation resources are also important in helping you succeed in the exam. These may include textbooks, practice exams, online resources, and study groups.
It’s recommended that you use a variety of resources to prepare adequately for the exam.
What is the cost to take the Fundamentals of Nursing Exam 1?
To take the Fundamentals of Nursing Exam 1, you’ll need to pay an exam fee. The cost of this fee may vary depending on where you take the exam, but you can expect to pay anywhere from $100 to $300.
Payment methods may also vary, but most testing centers accept credit cards, debit cards, and money orders. Some may also accept personal checks or cash, so be sure to check with the testing center beforehand to see what payment options are available.
Overall, it’s important to plan ahead and make sure you have the necessary funds to cover the exam fees before you schedule your test.
Conclusion
Congratulations! You’ve completed your comprehensive study of the fundamentals of nursing exam 1 PDF. By reading and understanding the materials covered in this guide, you’re now better equipped to tackle the challenging topics you may encounter in your nursing career.
Remember that nursing is a noble profession that requires patience, compassion, and dedication. As a nurse, it’s your duty to provide the best possible care to your patients and ensure their safety and well-being.
Always apply the nursing process, follow infection control protocols, and administer medications with caution.
Finally, keep learning and growing as a nurse. Best of luck in your nursing journey!